Mahajan Eye Hospital is one of the leading institutions in the diagnosis and treatment of keratoconus.
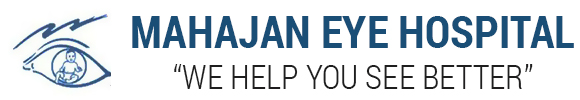
Keratoconus, often abbreviated to “KC”, is a non-inflammatory eye condition in which the normally round dome-shaped cornea progressively thins causing a cone-like bulge to develop. This results in significant visual impairment.
Who gets Keratoconus?
The actual incidence of KC is not known. It is not a common eye disease, but it is by no means rare. It has been estimated to occur in 1 out of every 2,000 persons in the general population. Keratoconus is generally first diagnosed in young people at puberty or in their late teens. It is found in all parts of the India and the rest of the world. It has no known significant geographic, cultural or social pattern.
What happens?
The cornea is the clear window of the eye and is responsible for refracting most of the light coming into the eye. Therefore, abnormalities of the cornea severely affect the way we see the world making simple tasks, like driving, watching TV or reading a book difficult.
In its earliest stages, keratoconus causes slight blurring and distortion of vision and increased sensitivity to light. These symptoms usually first appear in the late teens and early twenties. Keratoconus may progress for 10-20 years and then slow or stabilize. Each eye may be affected differently.
Keratoconus Treatment - Options Overview
What is Collagen Cross-Linking:
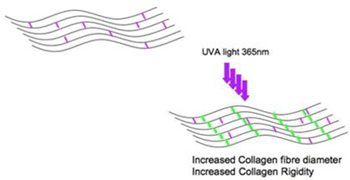
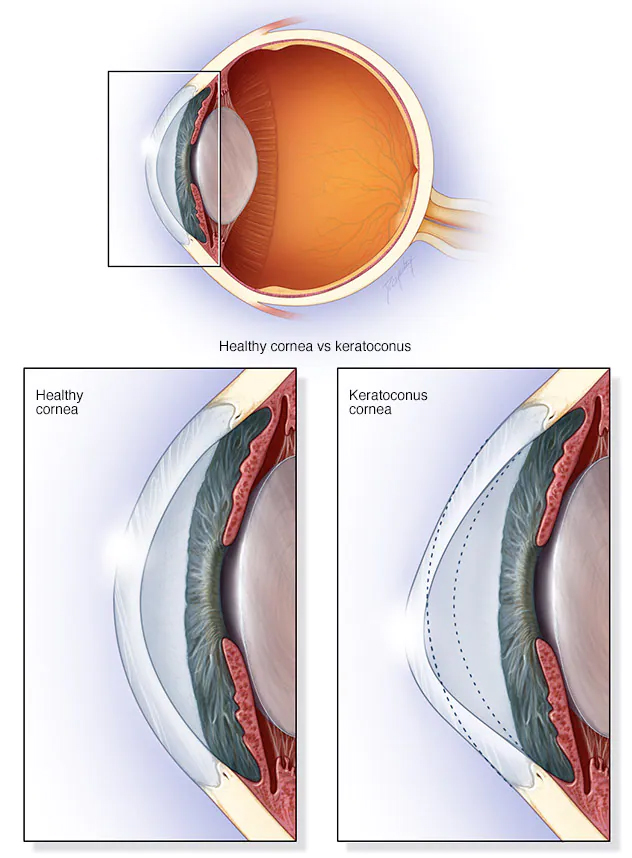
This is a procedure which increases the chemical bonding of the collagen fibres of the cornea thus helping to halt the progression of keratoconus.
The one hour C3-R treatment is performed in the hospital. During the treatment, custom-made riboflavin eye drops are applied to the cornea, which is then activated by ultraviolet light(370nm). This amazingly simple process has been shown in laboratory and clinical studies to increase the amount of collagen cross-linking in the cornea and strengthen the cornea. In published European studies, such treatments were proven safe and effective in patients.
We at Mahajan Eye Hospital have been successfully performing this procedure since the last 7 years.
How is the treatment done?
 The treatment involves removing the skin (epithelium) from the surface of the cornea and then applying Riboflavin eye drops. The eye is then exposed to UVA light for 30 minutes. After the treatment, an eye-pad is worn for 1-3 days and antibiotic ointment is applied to the treated eye four times a day until the surface of the eye has healed.
The treatment involves removing the skin (epithelium) from the surface of the cornea and then applying Riboflavin eye drops. The eye is then exposed to UVA light for 30 minutes. After the treatment, an eye-pad is worn for 1-3 days and antibiotic ointment is applied to the treated eye four times a day until the surface of the eye has healed.
Who can benefit from this treatment?
It is important to understand that collagen cross-linking treatment is not a cure for keratoconus. Rather, it aims to slow or even halt the progression of the condition. After the treatment, it is expected that it will continue to be necessary to wear spectacles or contact lenses (although a change in the prescription may be required). However, it is hoped that the treatment will prevent further deterioration in vision and the need for corneal transplantation.
What are the risks?
There are a number of potential risks associated with this treatment although very few complications have been reported so far.
Ultraviolet light is potentially harmful to the eye and some damage does occur to the cells in the front part of the cornea where the treatment has its effect. However, the dose used is designed to prevent observable damage to the cells that line the back of the cornea or the other structures within the eye. No lens opacities (cataracts) have been attributed to this treatment in European trials.
The treatment involves the scraping away of the outer layer (skin or epithelium) of the cornea. There is therefore a risk that the surface of the cornea will be slow or fail to heal.
Infection may occur which could lead to the development of corneal scarring. Antibiotics are routinely used to prevent this complication. Corneal scarring might necessitate further surgical procedures (including corneal transplantation).
Other lesser but more common risks include:
Inability to wear contact lenses for several weeks after the treatment. Changes in the shape of the cornea necessitating a refitting of a contact lens or a change in the spectacle correction.
The increased corneal rigidity induced by exposure to UVA and riboflavin may wear off over time and further periodic treatments may be required, raising the possibility of other side effects from repeat doses of the treatment.
A NEW FORM OF COMBINATION TREATMENT HAS BEEN INTRODUCED WHICH INVOLVES COLLAGEN CROSSLINKING AND INTACS AFTER 3-6 MONTHS. THIS TREATMENT IS KNOWN TO HALT THE PROGRESSION AND ALSO STABILISES THE CORNEA.
Restoring quality of life through better vision…
Intacs corneal implants is an FDA approved option for the keratoconus patient that is in-between contact lenses and a corneal transplant!
Keratoconus is a progressive eye disease, which causes a thinning of the cornea, the clear front surface of the eye. As keratoconus progresses, the quality of one’s vision deteriorates and contact lenses or glasses no longer become a satisfactory solution for most people. Historically, a corneal transplant has been the only option – until Intacs!
Intacs corneal implants are an exciting option for individuals experiencing an intolerance to contact lens and are facing a corneal transplant. Intacs corneal implants may be the best possible option to stabilize the cornea, improve vision and potentially defer the need for a corneal transplant.
Intacs corneal implants are indicated for use in the correction of nearsightedness and astigmatism associated with keratoconus where contact lenses and glasses are no longer suitable.
Intacs corneal implants are approved by the FDA for keratoconus under a Humanitarian Device Exemption (HDE).
The Intacs Corneal Implant Procedure
Prior to any surgical procedure it is common to experience a degree of anticipation and anxiety. It may be comforting to know that the Intacs procedure is far less invasive than a corneal transplant or many other surgical procedures of the eye and the Intacs success rate is high. The surgeons performing the procedure are typically corneal surgeons, having expertise with keratoconus. Each surgeon has also undergone a rigorous training program specific to Intacs for treating patients with keratoconus.
Before the Procedure
Typically, your ophthalmologist, possibly working in tandem with an optometrist will have you undergo a thorough eye examination. Your examination will include a variety of standard ophthalmic tests for this type of procedure, as well as general medical tests and a review of your specific medical history.
Anesthetic drops are used to numb the eye, which is held open throughout the procedure to prevent blinking.
Step 1: A single, small incision is made in the surface of the cornea.
Step 2: The eye is prepared for Intacs placement.
To stabilize your eye and ensure proper alignment of the Intacs inserts, the centering guide is placed on the surface of your eye. During this time, inner layers of the cornea are gently separated in a narrow circular area to allow for Intacs placement.
Step 3: The Intacs inserts are gently placed.
After the second Intacs insert is placed, the small opening in the cornea is closed.
Step 4: The procedure is completed.
The placement of Intacs inserts remodel and reinforce your cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide you with improved vision.
Follow-up visits will be required to monitor the healing process and evaluate the visual benefits of the procedure. Even after a successful procedure, glasses or contacts still may be required to provide you with good vision.
As with any surgical procedure, there are some risks, including infection. Some patients experience visual symptoms including difficulty with night vision, glare, halos, blurry and fluctuating vision.
Implantable Collamer Lens Service
There’s a big difference between “visual acuity” (6/6 vision is considered normal visual acuity) and “visual quality.” Many refractive procedures such as LASIK offer the promise of improved visual acuity but the quality of your vision may vary significantly based on the procedure you choose. The ICL provides vision correction that goes beyond LASIK. It helps you enjoy sharper, clearer, and more vivid vision, with greater depth and dimension.
When compared to other refractive surgical procedures, the ICL creates sharper vision. The immediate improvement of vision quality and the remarkably short and painless recovery produces a unique “WOW!” factor in patients.
The “High Definition Vision” delivered by the ICL makes this proven, technologically advanced vision correction procedure the choice for patients who need and expect high quality results. The ICL is clearly the choice for patients with an active lifestyle and those who cannot accept anything less than the highest quality vision.
If you can’t settle for “good enough” vision and demand “High Definition Vision,” the ICL is clearly the refractive procedure choice for you.
Guidelines to patients desiring ICL procedure:
- Are between the ages of 18 and 45 years.
- Are nearsighted or farsighted, including those with mild, moderate, and high power with or without occurrence of astigmatism. The Toric ICL™, capable of correcting myopia and astigmatism together and combines two procedures into one.
- Have proper anterior chamber depth and acceptable eye tissue cell density (this will be determined by the eye surgeon or ophthalmologist after a comprehensive eye exam).
- Have not had a change in their eyeglass prescription of more than 0.50 Diopters in 6 months.
- Are not currently pregnant.
- Have no known allergies to medications used during refractive surgery or no other contraindications.
- Have dry eyes, severe myopia, or a thin cornea (non-LASIK candidate).
Consultation
During your first examination we need to dilate your pupils using eye drops. Dilatation of the pupils may temporarily blur the vision of some people for a few hours. Therefore, we advise that you make arrangements for someone else to drive you back home. It would also help if you can get a pair of dark glasses along.
Eye examinations normally take time. You may have to spend an hour or more at the hospital. We would appreciate your patience.
As an ICL candidate, we will prepare your eyes one to two weeks prior to surgery by using a laser to create a small opening between the lens and the front chamber of your eye (Iridotomy). This allows fluid to pass between the two areas, thereby avoiding the build-up of intraocular pressure following the surgery. However, this can be done on the same day of the surgery.
Surgical Procedure
The implantation procedure for the ICL involves a procedure similar to that of cataract surgery but unlike cataract surgery, the ICL procedure does not require the removal of the eye’s crystalline lens. The entire procedure for the implantation of the ICL will take about 15 to 30 minutes. Most patients say it is relatively painless because of the numbing agents used. Please bring someone along to drive you home following the procedure.
Topical Anaesthesia: On the day of your procedure, prior to surgery, your surgeon will administer topical anaesthesia to minimize discomfort; however you may still feel pressure in your eye. Additionally, you may or may not be given a sedative.
Lens Positioning Openings: Once you are comfortable, your surgeon will begin the procedure. First, the surgeon will create one or two small openings at the base of your cornea that will be used to position the lens.
Gel-like Solution: Next, a gel-like substance will be placed inside your eye to protect the eye during lens placement. This gel will be removed at the end of the procedure.
Lens Opening: Following placement of the gel, a small opening will be made, through which the lens will be inserted.
Insertion of Corrective Lens: Prior to the ICL procedure, your corrective lens was selected based on your individual prescription. The lens was folded and loaded into a small cartridge which will now be placed through the incision. As the lens is inserted, it will gently unfold in your eye. Once the lens has fully unfolded, the four corners of the lens will be placed behind your iris. This makes the lens invisible to both you and others.
Completion of Procedure: To complete the procedure, the surgeon will administer eye drops to help prevent infection and inflammation. You will continue to use these drops for several days after your procedure.
Because the incision made during surgery is so small, sutures are typically not needed following the ICL surgery. For comfort and protection, the surgeon may cover the eye with a patch or shield and prescribe drops or medication.
You should not be able to drive immediately after the ICL surgery, so it is important that you arrange for transportation home.
Follow-Up Care after the ICL Procedure: Within 24 hours of undergoing the ICL surgery, you will have a follow-up visit with the ophthalmologist. The surgeon will monitor the eye’s internal pressure and will discuss your progress.
Patients need to follow physician instructions, especially regarding the needed use of antibiotics an anti-inflammatory medication during the week following the procedure.
Patients should contact their eye surgeon immediately if they experience severe eye pain or a sudden decrease in vision.
Baldeless Lasik
Mahajan Eye Hospital is the first and only hospital in PUNJAB to offer you the revolutionary Z-LASIK Z bladeless lasik treatment for spectacle removal. If you are looking for accurate, safe and comfortable laser refractive surgery, Z-LASIK Z is the procedure of choice for you.
Z-LASIK Z corrects your vision using laser surgery from the beginning to end. Z-LASIK Z is state of the art technology and the risk for complications is reduced even further and the quality of post-operative vision exceeds other methods and techniques. Have your vision corrected the gentle way and benefit from the most innovative technology for Laser Eye Surgery available today.
The FIRST compact, unique, mobile Femtosecond Surgical Lasers
Special Features of FEMTO LASER – Z6

- Lowest pulse energy (nJ range)
- Highest pulse repetition rate (Mhz)
- Shortest pulse width
- Tissue preservation
- Cleavage free tissue dissection
- Fewer to No gas bubbles
- Minimal mechanical stress
- Minimal side effects
- Quieter eyes, free of edema
- Truly safe for Ultra Thin corneal resections
Based on clinical experience from over 1.5 million successful Z-LASIK procedures, the FEMTO systems stand out as the femtosecond lasers with a remarkably low complication rate.
Now, you can choose TAILORED LASIK TREATMENT FOR PRESBYOPIA with Z6 BE ONE OF THE FIRST for Keratoconus treatment with Femtosecond Laser.
What is Z-LASIK?
Z-LASIK Z- is the gold standard in LASIK
(Lasik: Laser assisted in-situ keratomelusis) is the most advanced refractive procedure available that corrects near-sightedness and astigmatism by gently reshaping the cornea and changing the focusing ability of the eye. It reduces the Dependence on Glasses and Contact Lenses.
What is the difference between Z Lasik and INTRALASE I LASIK
Ziemer Z6 is the bladeless lasik machine of the future. Its performance is unparalleled by any other bladeless lasik system in the world. Consider a simple thing – the safety, efficiency and accuracy of a bladeless lasik system depends upon the frequency at which it operates. Intralase I LASIK systems operate at a frequency of 150 Khz and are sensitive to the room temperature, humidity and other environmental variables. The ZEISS bladeless system operates at a frequency of 500 Khz hence is more efficient and gentle to the eyes than intralase. The ZIEMER Z6 bladeless system operates at a frequency of 20000 (twenty thousand) Khz and hence is extremely safe, accurate and gentle on the eyes than the other systems. So, Z lasik system is 133 times better than Intralase LASIK and 40 times better than Zeiss system.
Z-LASIK®method – The Premium LASIK Procedure
LASIK vision correction is a two-step procedure
Step 1-Flap Creation
With FEMTO LDV™ laser
During the first step the femtosecond laser creates an ultra thin flap in the cornea by applying millions of tiny laser spots. Thanks to the laser this occurs precisely within one hundredth of a millimetre according to the requirements defined by earlier diagnostic tests. The need for a blade is eliminated – the whole procedure is completely blade-free! The flap, remaining hinged on one side, is then gently folded back and the eye is ready for step two.
Step 2-Vision Correction
With Excimer Laser
The final reshaping of the cornea is performed using an Excimer laser based on your refractive errors and desired visual outcome. After applying desired frequency of Laser on cornea, the flap is then replaced to its original position, where it adheres naturally. The entire procedure takes only a few minutes and is pain-free.
In conventional LASIK, a blade is used to make the flap. Z-LASIK however uses the FEMTO LDV™ femtosecond laser to create the flap. It makes the whole procedure completely blade-free and enables the surgeon to tailor the procedure according to the very unique characteristics of each patient. A truly personalized, painless and safe
With Z LASIk, the flap resection is created at the requested depth which results into
- Natural curvature flap edges
- Smooth, self-sealing flap edges
- Flaps can be easily lifted
- Truly customizable flap creation
- Excellent stroma bed quality
- No opaque bubble layer, or transient light sensitivity
What is the difference between a Corneal flap created with the Z Lasik and one created with INTRALASE
In traditional LASIK microkeratome cuts a thin, hinged flap into the eye’s clear surface (cornea). The microkeratome is a hand-held instrument, which contains a steel blade that moves back and forth and creates a cut as it travels across the cornea. A microkeratome is only capable of making a single, one-dimensional cut across the cornea. The flap then is lifted for application of laser energy that reshapes the eye for vision correction. Z Lasik directs laser energy precisely to create a thin, hinged flap, which then is lifted temporarily from the eye’s surface or cornea. In Z Lasik or Bladeless Lasik, the surgeon uses computer software to guide the Femtosecond Laser beam, which applies a series of tiny bubbles within the central layer of the cornea just beneath the surface of your eye. The resulting corneal flap is created at a precise depth and diameter ‘pre-determined by the surgeon’. With Z-LASIK Z you have the flexibility to really individualize the LASIK flap. This new Z-LASIK method performs the resection in a three-dimensional mode. Each flap can be customized to accommodate the desired geometry.
What are the Advantages of Z-Lasik?
The major advantage of Z-Lasik over conventional LASIK is that the entire vision correction treatment is performed by a laser. The use of a mechanical microkeratome using a blade to make an initial incision into the cornea is no longer required. LASIK using femto-seconds lasers has been available for more than 5 years, and more than 2 million LASIK procedures using the femto-second laser have been performed successfully all over the world. It provides the most accurate and safest treatment for your eyes.
Femto LDV™ femtosecond laser is manufactured by Ziemer Ophthalmic Systems AG. For more information, please visit www.ziemergroup.com.
Frequently asked questions
Candidates for the ICL are between 21 and 45 years of age, suffer from myopia (nearsightedness), hyperopia (farsightedness) and or astigmatism and want to experience superior vision correction.
Nearly anyone seeking clearer vision may be a ICL candidate, including those with special or extreme vision correction needs. Please make an appointment if you wish to learn more about the procedure our consultants would be happy to answer your queries.
Women who are pregnant or nursing should wait to have the ICL implanted.
The Toric ICL is a variant of ICL. Toric ICL corrects your nearsightedness as well as your astigmatism (cylindrical power) in one single procedure. Each lens is custom made to meet the needs of each individual eye.
Prior to being placed on the market, the ICL was subject to extensive research and development. Today, more than 65,000 patients worldwide enjoy the benefits of the device. In an USFDA clinical trial, over 99 percent of patients were satisfied with their implant. The ICL has a record of stable, consistently excellent clinical outcomes. The lens has been available internationally for over 12 years.
No, most patients state that they are very comfortable throughout the procedure. We use a topical anesthetic drop prior to the procedure and sometimes may choose to administer a light sedative as well.
The ICL is made of Collamer®, a highly biocompatible advanced lens material which contains a small amount of purified collagen. Collamer does not cause a reaction inside the eye and it contains an ultraviolet filter that provides protection to the eye.
The ICL allows extreme flexibility of treatment options. If your vision changes dramatically after receiving the implant, it can be removed and replaced. If necessary, another procedure can be performed at any time.
Patients can wear glasses or contact lenses as needed following treatment with the ICL. The implant does not treat Presbyopia (difficulty with reading in people 40 and older), but you can use reading glasses as needed after receiving the ICL.
No, the ICL is positioned behind the iris (the coloured part of the eye), where it is invisible to both you and observers. Only your doctor will be able to tell that vision correction has taken place.
The ICL is designed to be completely unobtrusive after it is put in place. It stays in position by itself and does not interact with any of the eye’s structures
Researchers estimate that keratoconus affects 1 in 2000 people. The disease affects men and women alike and there are no known differences between races. Although the cause of the disease is unknown, research has suggested that genetics, allergies and other environmental factors may contribute to the onset of the disease.
Initially, a person with early stage keratoconus will notice a subtle change in their vision. As the disease progresses, one’s vision will fluctuate and frequent changes to one’s glasses or contact lenses often occur. This happens as a result of a thinning taking place within the cornea and bulging caused by one’s normal eye pressure pushing on the weakened front surface of the eye. As the disease continues to advance, the light rays entering the eye become significantly distorted, called irregular astigmatism. The outer portion of the eye begins to bulge, creating what often looks like a cone shape.
Yes, in approximately 90% of keratoconus cases the disease will manifest itself in both eyes. The rate of progression and the timing of the onset of the disease is typically different for each eye.
The onset of keratoconus can occur anywhere between the ages of 8 to 45. In the majority of the cases, it becomes apparent during the teen years and slowly worsens before stabilizing somewhat in the 30’s or 40’s.
Typically, an eyecare professional will treat early stage keratoconus with contact lenses or glasses addressing the early vision correction needs of the patient. In later stages, rigid gas permeable contact lenses are often recommended. These lenses are used to improve one’s vision and to brace the bulge in the cornea. In advanced cases, where the patient can no longer achieve adequate functional vision with contact lenses, corneal transplant surgery may be necessary.
o, historically very few if any persons suffer from total blindness from keratoconus alone. But in severe cases, one’s vision can be significantly impaired and normal everyday activities may be difficult.
Due to the onset and progression of keratoconus, the weakened cornea looses its natural dome-like shape. As a result, the light rays entering the eye are no longer focused properly, impairing one’s ability to see images clearly.
Intacs are specially designed inserts, made of medical plastic, which are surgically placed under the surface of the cornea. Due to their unique patented design, Intacs are able to remodel the architecture of the cornea re-establishing a more natural dome-like shape and improving one’s vision.
Of those who suffer from keratoconus, approximately 20% will undergo a corneal transplant. The success rate is high although the grafts only last for about 10 years, therefore a young person may have to undergo several corneal transplants. The recovery time for the patient varies and can take more than a year. Contact lenses or glasses are typically required after surgery to achieve acceptable vision.
A corneal transplant is an invasive surgical procedure, requiring the removal of a section of your cornea and having it replaced with donor tissue. Although successful, it is a delicate procedure with typically a long recovery period.
The Intacs procedure does not require removal of corneal tissue, but rather works on the principle of reshaping your own cornea from within utilizing special designed corneal inserts that provide structure to a weakened cornea. The recovery period is typically short, with visual improvement noticed almost immediately.
In the few cases in which a corneal transplant was performed after an Intacs procedure, there were no complications reported.